In this article, I’ll try to give you a good overview of stress fractures generally, as well as giving you a little insight into my mind (scary place to be I know!) when I’m reasoning through how to manage a stress fracture, as there are a number of variables to be aware of.
So if you’re sitting comfortably, we shall begin…
A stress fracture is essentially a crack or break in the bone. It differs from a standard fracture by way of mechanism.
Standard fractures are usually caused by a sudden, severe, high force trauma, like a fall from a great height, or a road traffic accident.
Stress fractures, on the other hand, are the result of an accumulation of sub-maximal loading over time. So the forces experienced are not great enough to break the bone outright, but the repeated application of that stress, without adequate recovery is enough for the bone to fail.
Now, I don’t want anyone reading this to worry about running and the health of your bones: Your bones are organic tissue and respond brilliantly to loading. So running is generally great for bone health.
When you load a bone, like in running, and give it sufficient recovery, it undergoes a process of re-absorption and bone formation that ultimately strengthens the bone.
If however, repeated load is placed on the bone, without sufficient recovery time in between, the bone doesn’t have the time to strengthen before the next bout of loading is applied. When this happens regularly, a stress fracture can result.
This is another great example of ignoring the law of adaptation and doing too much too soon. The cardinal sign of most running injuries!
The mechanism of stress fractures can be split into 4 camps:
Traction (muscles and connective tissue pulling on the bone repeatedly/excessively), impact, rotation or a combination of the above. Most running stress fractures are impact related, with the fractured bone having to absorb the the repetitive ground reaction force.
Fig 1. shows the progression of bone stress.
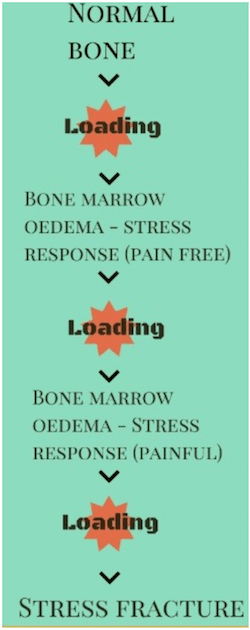
Fig. 1: Stages of bone stress leading to stress fracture
Signs & Symptoms
You can have a stress fracture in any bone, but it tends to effect the weight bearing bones in runners.
Common areas include:
- 2nd and 5th metatarsals
- Tibia
- Fibula
- Navicular
- Neck of femur
Diagnosing stress fractures
A big part of diagnosing stress factors, is in the subjective history, or the story the patient tells you.
In runners, there is traditionally a story that involves a change in training. This can be a sharp increase in mileage, or increase in intensity, such as adding in a new plyometric programme.
It could be as simple as a change in footwear but there is usually a change somewhere.
The location of pain, tends to be very local to the area of the fracture. There is often some swelling present too. In the early stages of the condition the pain is felt on weight bearing and is activity related, so pain is felt on running and worsens the more you do. As the condition progresses, the pain is there even at rest and often manifests at night.
Physical tests that can help diagnosis include palpation (touching in and around the painful area), as mentioned above, you would expect quite a local area of pain, not a widespread, diffuse pattern. Impact tests, although a bit cruel, can help with diagnosis. These include hopping, jumping and stamping and you’re basically looking for reproduction of the patients symptoms. These are often used as objective markers, a way to measure progress, so once they are pain free it’s a good sign that you’re ready to progress.
From an imaging perspective, MRI is the method of choice for diagnosing stress fractures.
Prevention / How to manage stress fractures
If I’ve reached the diagnosis of a stress fracture, the next question is: How are we going to manage it?
Not all stress fracture are made equal, so at this stage I have a few things going through my mind:
- Is it a high risk fracture?
- What are pain levels like? and how irritable is it?
- What is the quality of the bone like in the first place?
- Biomechanics
Is it a high risk stress fracture?
A high risk stress fracture, is a stress fracture with a high risk of non-union or delayed healing. Any area that has a poor blood supply, or risk of developing into a full fracture, can be classified as high risk.
A high risk fracture is managed with either surgery or at the very aggressive end of conservative management (see fig.2).
High risk fractures include:
- Neck of femur: Tension side (In certain fractures you get a tension side and a compressive side. In the compressive side, as the name suggests, the bones are being pushed together so actually favours union and healing, whereas the tension side is repeatedly being pulled apart, so it can be difficult for that area to heal and unite).
- The patella
- Medial malleolus
- The base of the 5th metatarsal
- Navicular
- Sesamoid bones of the big toe
Pain levels & Irritability?
Having taken on board whether the stress fracture is high or low risk (most running stress fractures are low risk) you can then use pain levels, and how much activity it takes to bring on the pain, as guidance on how aggressively you need to offload.
Intuitively, we need the area to heal. Luckily, all that wisdom is already in your body. All you have to do is give it the right environment to heal in. This means taking the load off the injured area to give it a chance to do this.
In the lower risk stress fractures, you only need to back off activity, to pain free levels. It’s wise to maintain the strength and health of adjacent body parts, so there’s nothing wrong with training the other joints, other leg, or upper body, whilst waiting for the injured area to heal.
You may also cross train, as long as it’s pain free. Common examples are cycling and pool running. I’m a big fan of deep water pool running when you’re injured. You can maintain good running mechanics and still get all the physiological benefits of your run, just without the load!
So, if you work at the right intensity, you can still do a lactate threshold workout in the pool.
Bottom line is, if you understand stress fractures (which hopefully this article is going a long way to helping) and have been cleared of a high risk stress fracture, then there’s still loads you can do to maintain, and even further, your fitness.
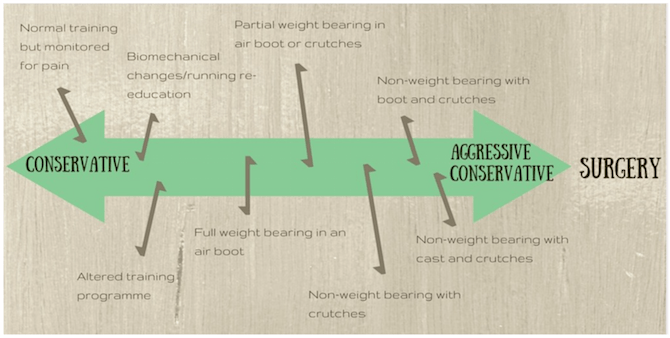
Figure 2: A continuum of conservative offloading.
Conservative or Aggressive Conservative?
What’s the quality of the bone like in the first place?
Clearly, if you have a higher bone density i.e. stronger bones, that bone is less likely to develop a stress fracture and be better able to withstand the repetitive forces of running.
New runners, especially if there has been no other history of regular weight bearing exercises, tend to have less dense bone tissue, compared to runners who have been running and exercising regularly over years.
Poor nutrition and low vitamin D, have also been associated with poor bone health and therefore could put you at a higher risk of a stress fracture.
Women, with what known as the female athletic triad (eating disorders, amenorrhoea and osteoporosis) are also likely to have poorer bone health. It’s been reported that stress fractures in athletes with menstrual disturbances is 2 to 4 times that of eumenorrheic athletes.
A lack of oestrogen (or testosterone in men) has been related to poor bone health.
These issues are important to know, and with the help of a nutritionist or consultant, supplementation or medication can form part of the management plan.
Biomechanics
The last thing whizzing around my brain at this point, is biomechanics. Biomechanics don’t necessarily cause a stress fracture, but they can give us the clues as to “why there?“.
I’m always fascinated why runners come in with pain that manifests in different areas. Why does runner ‘X’ have a stress fracture in his tibia and runner ‘Y’ have a stress fracture in his 5th metatarsal?
Likewise, why does runner ‘A’ have illiotibial band syndrome and runner ‘B’ have plantar fasciitis?
They’re all, likely, guilty of too much too soon, but biomechanical analysis (a posh word for just looking at how you move), gives us an insight into why that particular area has been overloaded.
It may be enough, just to offload the area until pain free, and then just be more graded with your mileage and intensity to prevent further problems. However, some people may benefit from a slight change in running technique to decrease load on that area.
Let me give you a couple of examples of how I change running technique and my reasoning behind each one:
Example 1: Tibial stress fracture
The cues I tend to use here, to offload the anterior medial tibia, are similar to that of medial tibial stress syndrome (MTSS) (some people believe tibial stress fractures and MTSS are on a continuum anyway, so it makes sense)
- Increase cadence: One of my most used running re-education cues across the board. The best way to do this is via the use of a metronome. There are lots of free metronome apps if you have an iPhone, or you can by one pretty cheaply from places like Amazon. There’s no set stride rate you should aim for, so have a play around with it a bit. Generally, I go for 5%-10% more than your current cadence at a given pace and see what happens. You can always gradually increase it from there and re-assess the ‘experiment’. The theory behind increasing your cadence is to decreased an over stride, get you landing closer to your centre of mass (CoM) and with a straight tibia, as opposed to your tibia flicking out ahead of the knee. Think of it a bit like a pole vaulters pole. As they approach the jump, they plant the pole ahead of themselves so you see this big, anterior bowing of the pole, great for pole vaulting but not so good for tibias! If you can imagine the pole vaulter placing the pole down vertically, and not ahead of themselves, you will see a pretty crappy pole vaulter, but also less anterior bowing of the pole, that’s what we are looking for: less anterior bowing = less force through the painful area.
- Increase step width: Trying to move the load from the medial shin to achieve less varus (side bending) tibial bowing. I try and bring about this change using a variety of cues, and what works for one doesn’t always work for the next. Generally, asking people to have some daylight between their legs, imagine running on either side of a yellow parking line or, recently, i’ve been getting my runners to run with a resistance loop just above their knees, and instruct them to keep the pressure on the band.
- Stiffen the ankle: The idea here is to decrease the amount of dorsiflexion the ankle goes through. Lessening dorsiflexion, means less tibial bowing from the action of soleus as it tries to decelerate the tibia. Stiffening the ankle also helps to pretension the muscles so they can work reactively and elastically. Good for speed but also takes the load of the bone itself.
- Change the direction of the ground reaction force: Again, we are trying to decrease the anterior tibia bowing. If we go back to our rubbish pole vaulter, as we discussed, if he places the pole out in front of him with forward and downwards force it will create anterior bowing, however, if he plants the pole down with a backward and downwards force, it will not bow anteriorly, but posteriorly i.e the force will go more through the back of the tibia. Any change in the direction of the ground reaction force to a more backwards and downwards force will decrease the load in the anterior tibia and may be enough for us to keep running without pain. To cue this, I often video them and freeze the frame of them running when their swing leg is at its highest. From this position I instruct them to push their leg back and down, in a backwards tick type direction, using their glutes to perform the movement. Sometimes i’ll ask them to paw back on the ground (bit of a controversial cue from a performance perspective, but can just get them to direct the force more backward and down).
- Posture: Encourage the patient to run up tall. I often use the ‘helium balloon attached to the crown of the head’ cue. This cue helps decrease an anterior pelvic tilt or a forward lean from the waist. Both of these mechanics lead to the centre of mass shifting forwards. To compensate for this, you will have to over stride with the next step = more load on knee and shin area.
Example 2: 2nd metatarsal stress fracture
There could be a few reasons why the 2nd metatarsal is being overloaded. For simplicity, let’s say that gait analysis showed, generally good biomechanics higher up, but a pronounced forefoot strike. This would put a lot of stress through the metatarsals so would be a good idea to change.
You could work on the “oranges cue” (I have to give credit where it’s due, this cue was taken from the excellent Dr. Andy Franklyn-Miller and John Foster).
Basically, the idea of the “oranges cue” is to imagine that you have an orange taped to the bottom of your foot, around the mid arch area. Your goal is to squash the orange, without letting the orange squirt out the front (heel strike) or back (fore foot strike). As you’ve probably worked out, this will encourage a more mid-foot strike pattern.
Once you have all the above information, you should have enough data to make a decision as to how you’re going to manage this stress fracture, and, where on the management continuum you are going to begin (Conservative? Aggressive Conservative? Somewhere in between?).
Use your objective markers (hopping, jumping, stamping) along the way, to assess progress.
Stress fractures can take anywhere between 4 to 12 weeks to recover so, as always, I firmly believe that prevention is better than cure.
Stress fractures rarely surprise you out of the blue, there are warning signs along the way. Without going too deep in a running article, you’re body has great wisdom, if you listen to what it’s telling you, it will guide you to the right path.
The post Understanding Stress Fractures in Runners appeared first on Run Coaching, Ironman and Triathlon Specialists - Kinetic Revolution.
from Run Coaching, Ironman and Triathlon Specialists - Kinetic Revolution http://feedproxy.google.com/~r/KineticRev/~3/i8kCzeuWZ2w/

No comments:
Post a Comment